what are the paddles called used to resuscitate
| Defibrillation | |
|---|---|
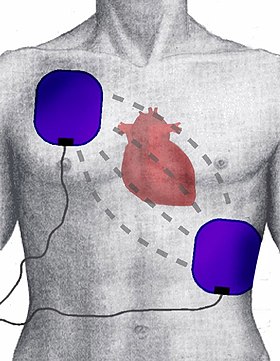 View of defibrillator electrode position and placement |
Defibrillation is a handling for life-threatening cardiac dysrhythmias, specifically ventricular fibrillation (VF) and non-perfusing ventricular tachycardia (VT).[1] [two] A defibrillator delivers a dose of electric current (oftentimes called a counter-daze) to the heart. Although not fully understood, this procedure depolarizes a big corporeality of the center muscle, ending the dysrhythmia. Subsequently, the torso'southward natural pacemaker in the sinoatrial node of the heart is able to re-establish normal sinus rhythm.[3] A heart which is in asystole (flatline) cannot be restarted past a defibrillator, but would be treated by cardiopulmonary resuscitation (CPR).
In dissimilarity to defibrillation, synchronized electrical cardioversion is an electric shock delivered in synchrony to the cardiac cycle.[four] Although the person may still be critically ill, cardioversion normally aims to end poorly perfusing cardiac dysrhythmias, such every bit supraventricular tachycardia.[1] [ii]
Defibrillators tin exist external, transvenous, or implanted (implantable cardioverter-defibrillator), depending on the type of device used or needed.[5] Some external units, known as automated external defibrillators (AEDs), automate the diagnosis of treatable rhythms, meaning that lay responders or bystanders are able to use them successfully with trivial or no grooming.[two]
Utilize of defibrillators [edit]
Indications
Defibrillation is frequently an important step in cardiopulmonary resuscitation (CPR).[6] [7] CPR is an algorithm-based intervention aimed to restore cardiac and pulmonary part.[half dozen] Defibrillation is indicated merely in certain types of cardiac dysrhythmias, specifically ventricular fibrillation (VF) and pulseless ventricular tachycardia.[1] [2] If the center has completely stopped, as in asystole or pulseless electric activity (PEA), defibrillation is not indicated. Defibrillation is also not indicated if the patient is conscious or has a pulse. Improperly given electrical shocks can cause dangerous dysrhythmias, such as ventricular fibrillation.[one]
Application method
The defibrillation device that is unremarkably bachelor out of the medical centres is the automated external defibrillator (AED),[8] a portable machine that tin exist used fifty-fifty by users with no previous training. That is possible considering the machine produces pre-recorded voice instructions that guide to the user, and automatically checks the victim's status and applies the correct electric shocks. Anyway, there besides exist written instructions of defibrillators that explicate the procedure footstep-past-step.
Outcomes
Survival rates for out-of-hospital cardiac arrests are poor, often less than x%.[ix] Outcome for in-infirmary cardiac arrests are higher at xx%.[9] Within the grouping of people presenting with cardiac arrest, the specific cardiac rhythm tin can significantly touch on survival rates. Compared to people presenting with a non-shockable rhythm (such equally asystole or PEA), people with a shockable rhythm (such equally VF or pulseless ventricular tachycardia) have improved survival rates, ranging between 21 and 50%.[6] [10] [11]
Types [edit]
Transmission models [edit]
Transmission external defibrillators require the expertise of a healthcare professional.[12] [thirteen] They are used in conjunction with an electrocardiogram, which can be split up or built-in. A healthcare provider start diagnoses the cardiac rhythm and then manually determine the voltage and timing for the electrical shock. These units are primarily plant in hospitals and on some ambulances. For instance, every NHS ambulance in the United kingdom is equipped with a manual defibrillator for use by the attention paramedics and technicians.[ citation needed ] In the United States, many advanced EMTs and all paramedics are trained to recognize lethal arrhythmias and evangelize appropriate electrical therapy with a manual defibrillator when advisable.[ citation needed ]
An internal defibrillator is often used to defibrillate the eye during or subsequently cardiac surgery such every bit a middle bypass. The electrodes consist of round metallic plates that come in direct contact with the myocardium. Transmission internal defibrillators deliver the shock through paddles placed directly on the heart.[1] They are generally used in the operating room and, in rare circumstances, in the emergency room during an open heart procedure.
Automated external defibrillators [edit]
Automated external defibrillators (AEDs) are designed for utilize by untrained or briefly trained laypersons.[fourteen] [fifteen] [16] AEDs contain technology for analysis of heart rhythms. As a result, it does not require a trained health provider to decide whether or not a rhythm is shockable. By making these units publicly bachelor, AEDs have improved outcomes for sudden out-of-hospital cardiac arrests.[14] [fifteen]
Trained wellness professionals take more limited use for AEDs than manual external defibrillators.[17] Contempo studies show that AEDs does not better result in patients with in-hospital cardiac arrests.[17] [18] AEDs accept gear up voltages and does not allow the operator to vary voltage according to need. AEDs may also delay delivery of effective CPR. For diagnosis of rhythm, AEDs oftentimes require the stopping of chest compressions and rescue animate. For these reasons, certain bodies, such as the European Resuscitation Council, recommend using transmission external defibrillators over AEDs if manual external defibrillators are readily bachelor.[18]
Every bit early defibrillation can significantly ameliorate VF outcomes, AEDs have become publicly available in many easily accessible areas.[17] [eighteen] AEDs have been incorporated into the algorithm for basic life support (BLS). Many outset responders, such as firefighters, policemen, and security guards, are equipped with them.
AEDs can be fully automated or semi-automatic.[19] A semi-automatic AED automatically diagnoses middle rhythms and determines if a shock is necessary. If a shock is advised, the user must then button a button to administer the stupor. A fully automated AED automatically diagnoses the heart rhythm and advises the user to stand dorsum while the shock is automatically given. Some types of AEDs come up with advanced features, such as a manual override or an ECG brandish.
Cardioverter-defibrillators [edit]
Implantable cardioverter-defibrillators, also known as automated internal cardiac defibrillator (AICD), are implants like to pacemakers (and many can as well perform the pacemaking function). They constantly monitor the patient'southward eye rhythm, and automatically administer shocks for various life-threatening arrhythmias, according to the device's programming. Many mod devices tin can distinguish between ventricular fibrillation, ventricular tachycardia, and more benign arrhythmias like supraventricular tachycardia and atrial fibrillation. Some devices may try overdrive pacing prior to synchronised cardioversion. When the life-threatening arrhythmia is ventricular fibrillation, the device is programmed to proceed immediately to an unsynchronized stupor.
In that location are cases where the patient's ICD may burn down constantly or inappropriately. This is considered a medical emergency, as it depletes the device's battery life, causes significant discomfort and anxiety to the patient, and in some cases may actually trigger life-threatening arrhythmias. Some emergency medical services personnel are now equipped with a ring magnet to place over the device, which effectively disables the shock part of the device while nonetheless allowing the pacemaker to function (if the device is so equipped). If the device is shocking frequently, but appropriately, European monetary system personnel may administer sedation.
A wearable cardioverter defibrillator is a portable external defibrillator that can exist worn past at-risk patients.[20] The unit monitors the patient 24 hours a day and can automatically deliver a biphasic shock if VF or VT is detected. This device is mainly indicated in patients who are not immediate candidates for ICDs.[21]
Interface [edit]
The connection between the defibrillator and the patient consists of a pair of electrodes, each provided with electrically conductive gel in order to ensure a expert connectedness and to minimize electric resistance, also called breast impedance (despite the DC belch) which would fire the patient. Gel may exist either wet (similar in consistency to surgical lubricant) or solid (similar to gummi candy). Solid-gel is more convenient, considering there is no demand to clean the used gel off the person's skin after defibrillation. However, the apply of solid-gel presents a higher hazard of burns during defibrillation, since moisture-gel electrodes more evenly behave electricity into the trunk. Paddle electrodes, which were the outset blazon developed, come without gel, and must take the gel applied in a split footstep. Self-agglutinative electrodes come prefitted with gel. There is a general division of opinion over which type of electrode is superior in hospital settings; the American Heart Clan favors neither, and all mod manual defibrillators used in hospitals allow for swift switching between self-adhesive pads and traditional paddles. Each type of electrode has its merits and demerits.
Paddle electrodes [edit]

An automatic external defibrillator: this model is a semi-automatic due to the presence of a stupor button

The same AED with electrodes fastened
The most well-known blazon of electrode (widely depicted in films and television set) is the traditional metal "hard" paddle with an insulated (usually plastic) handle. This type must be held in identify on the patient's peel with approximately 25 lbs (11.3 kg) of force while a shock or a series of shocks is delivered. Paddles offering a few advantages over self-adhesive pads. Many hospitals in the United States continue the utilise of paddles, with disposable gel pads fastened in most cases, due to the inherent speed with which these electrodes can be placed and used. This is disquisitional during cardiac arrest, as each 2d of nonperfusion means tissue loss. Modern paddles permit for monitoring (electrocardiography), though in infirmary situations, carve up monitoring leads are oft already in place.
Paddles are reusable, being cleaned after employ and stored for the next patient. Gel is therefore non preapplied, and must be added earlier these paddles are used on the patient. Paddles are mostly only found on manual external units.
Self-adhesive electrodes [edit]
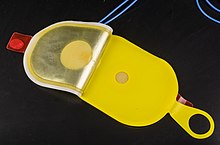
Self-adhesive electrodes of a defibrillator
Newer types of resuscitation electrodes are designed every bit an adhesive pad, which includes either solid or wet gel. These are peeled off their backing and practical to the patient's chest when deemed necessary, much the same as whatever other sticker. The electrodes are then connected to a defibrillator, much as the paddles would be. If defibrillation is required, the machine is charged, and the shock is delivered, without whatever need to utilize any additional gel or to retrieve and place whatever paddles. Most adhesive electrodes are designed to be used not only for defibrillation, but also for transcutaneous pacing and synchronized electrical cardioversion. These adhesive pads are institute on most automated and semi-automated units and are replacing paddles entirely in non-hospital settings. In hospital, for cases where cardiac abort is probable to occur (but has non notwithstanding), self-agglutinative pads may be placed prophylactically.
Pads besides offer an advantage to the untrained user, and to medics working in the sub-optimal conditions of the field. Pads practise not require extra leads to be attached for monitoring, and they do not require any force to be applied as the shock is delivered. Thus, adhesive electrodes minimize the run a risk of the operator coming into physical (and thus electrical) contact with the patient as the daze is delivered past allowing the operator to be upwards to several feet away. (The take a chance of electric daze to others remains unchanged, as does that of shock due to operator misuse.) Self-agglutinative electrodes are unmarried-employ only. They may exist used for multiple shocks in a single course of treatment, but are replaced if (or in case) the patient recovers then reenters cardiac abort.
Special pads are used for children under the age of eight or those under 55 lbs. (22 kg).[22]
Placement [edit]

Anterior-apex placement of electrodes for defibrillation
Resuscitation electrodes are placed according to one of two schemes. The anterior-posterior scheme is the preferred scheme for long-term electrode placement. One electrode is placed over the left precordium (the lower part of the chest, in front of the heart). The other electrode is placed on the back, behind the centre in the region between the scapula. This placement is preferred because it is best for not-invasive pacing.
The inductive-noon scheme (anterior-lateral position) can be used when the anterior-posterior scheme is inconvenient or unnecessary. In this scheme, the anterior electrode is placed on the correct, below the clavicle. The noon electrode is applied to the left side of the patient, just beneath and to the left of the pectoral muscle. This scheme works well for defibrillation and cardioversion, too as for monitoring an ECG.
Researchers take created a software modeling arrangement capable of mapping an individual's chest and determining the best position for an external or internal cardiac defibrillator.[23]
Mechanism [edit]

Defibrillator with pad positions shown: the model is biphasic and either pad can be placed in each position
The exact machinery of defibrillation is not well understood.[2] [24] One theory is that successful defibrillation affects most of the center, resulting in insufficient remaining heart musculus to continue the arrhythmia.[2] Contempo mathematical models of defibrillation are providing new insight into how cardiac tissue responds to a potent electrical shock.[24]
History [edit]
Defibrillators were first demonstrated in 1899 by Jean-Louis Prévost and Frédéric Batelli, two physiologists from the Academy of Geneva, Switzerland. They discovered that pocket-sized electrical shocks could induce ventricular fibrillation in dogs, and that larger charges would contrary the condition.[25] [26]
In 1933, Dr. Albert Hyman, middle specialist at the Beth Davis Hospital of New York Metropolis and C. Henry Hyman, an electrical engineer, looking for an alternative to injecting powerful drugs directly into the heart, came upward with an invention that used an electrical shock in place of drug injection. This invention was called the Hyman Otor where a hollow needle is used to laissez passer an insulated wire to the heart area to evangelize the electric shock. The hollow steel needle acted as one stop of the circuit and the tip of the insulated wire the other end. Whether the Hyman Otor was a success is unknown.[27]
The external defibrillator, as it is known today, was invented by electrical engineer William Kouwenhoven in 1930. Kouwenhoven studied the relationship between electric shocks and their furnishings on the human heart when he was a educatee at Johns Hopkins University School of Engineering. His studies helped him invent a device to externally jump start the heart. He invented the defibrillator and tested information technology on a canis familiaris, similar Prévost and Batelli. The start use on a human was in 1947 past Claude Brook,[28] professor of surgery at Case Western Reserve Academy. Beck'southward theory was that ventricular fibrillation oft occurred in hearts that were fundamentally salubrious, in his terms "Hearts that are too good to die", and that at that place must exist a style of saving them. Beck showtime used the technique successfully on a 14-year-old boy who was being operated on for a congenital breast defect. The boy's chest was surgically opened, and manual cardiac massage was undertaken for 45 minutes until the arrival of the defibrillator. Beck used internal paddles on either side of the heart, along with procainamide, an antiarrhythmic drug, and accomplished return of a perfusing cardiac rhythm.[ citation needed ]
These early defibrillators used the alternating current from a power socket, transformed from the 110–240 volts available in the line, up to betwixt 300 and 1000 volts, to the exposed heart past way of "paddle" blazon electrodes. The technique was often ineffective in reverting VF while morphological studies showed damage to the cells of the heart muscle postal service-mortem. The nature of the AC machine with a big transformer also made these units very hard to transport, and they tended to exist large units on wheels.[ citation needed ]
Closed-chest method [edit]
Until the early 1950s, defibrillation of the center was possible merely when the chest cavity was open during surgery. The technique used an alternate voltage from a 300 or greater volt source derived from standard Air conditioning ability, delivered to the sides of the exposed heart by "paddle" electrodes where each electrode was a flat or slightly concave metal plate of about forty mm diameter. The airtight-chest defibrillator device which applied an alternating voltage of greater than 1000 volts, conducted by means of externally applied electrodes through the chest cage to the heart, was pioneered by Dr 5. Eskin with assistance past A. Klimov in Frunze, USSR (today known as Bishkek, Kyrgyzstan) in the mid-1950s.[29] The elapsing of Air-conditioning shocks was typically in the range of 100-150 milliseconds[thirty]
Straight current method [edit]

A circuit diagram showing the simplest (non-electronically controlled) defibrillator design, depending on the inductor (damping), producing a Lown, Edmark or Gurvich Waveform
Early successful experiments of successful defibrillation by the discharge of a capacitor performed on animals were reported by N. Fifty. Gurvich and 1000. S. Yunyev in 1939.[31] In 1947 their works were reported in western medical journals.[32] Serial production of Gurvich's pulse defibrillator started in 1952 at the electromechanical constitute of the institute, and was designated model ИД-1-ВЭИ (Импульсный Дефибриллятор 1, Всесоюзный Электротехнический Институт, or in English, Pulse Defibrillator 1, All-Union Electrotechnical Found). It is described in particular in Gurvich'southward 1957 book, Middle Fibrillation and Defibrillation.[33]
The beginning Czechoslovak "universal defibrillator Prema" was manufactured in 1957 by the visitor Prema, designed by dr. Bohumil Peleška. In 1958 his device was awarded Grand Prix at Expo 58.[34]
In 1958, US senator Hubert H. Humphrey visited Nikita Khrushchev and amid other things he visited the Moscow Constitute of Reanimatology, where, amidst others, he met with Gurvich.[35] Humphrey immediately recognized importance of reanimation research and after that a number of American doctors visited Gurvich. At the aforementioned time, Humphrey worked on establishing of a federal program in the National Institute of Health in physiology and medicine, telling to the Congress: "Let's compete with United states of americaS.R. in inquiry on reversibility of death".[36]
In 1959 Bernard Lown commenced research in his beast laboratory in collaboration with engineer Barouh Berkovits into a technique which involved charging of a bank of capacitors to approximately 1000 volts with an energy content of 100-200 joules then delivering the charge through an inductance such as to produce a heavily damped sinusoidal wave of finite duration (~5 milliseconds) to the heart by style of paddle electrodes. This team further adult an understanding of the optimal timing of shock commitment in the cardiac cycle, enabling the application of the device to arrhythmias such every bit atrial fibrillation, atrial flutter, and supraventricular tachycardias in the technique known as "cardioversion".
The Lown-Berkovits waveform, as information technology was known, was the standard for defibrillation until the late 1980s. Earlier in the 1980s, the "MU lab" at the University of Missouri had pioneered numerous studies introducing a new waveform called a biphasic truncated waveform (BTE). In this waveform an exponentially decomposable DC voltage is reversed in polarity well-nigh halfway through the shock fourth dimension, then continues to disuse for some time after which the voltage is cut off, or truncated. The studies showed that the biphasic truncated waveform could be more efficacious while requiring the commitment of lower levels of energy to produce defibrillation.[xxx] An added do good was a pregnant reduction in weight of the motorcar. The BTE waveform, combined with automatic measurement of transthoracic impedance is the basis for mod defibrillators[ citation needed ].
Portable units [edit]

Wall-mounted emergency defibrillator
A major breakthrough was the introduction of portable defibrillators used out of the hospital. Already Peleška's Prema defibrillator was designed to exist more portable than original Gurvich'south model. In Soviet Union, a portable version of Gurvich'due south defibrillator, model ДПА-three (DPA-three), was reported in 1959.[37] In the west this was pioneered in the early on 1960s by Prof. Frank Pantridge in Belfast. Today portable defibrillators are among the many very important tools carried by ambulances. They are the only proven style to resuscitate a person who has had a cardiac arrest unwitnessed past Emergency Medical Services (EMS) who is still in persistent ventricular fibrillation or ventricular tachycardia at the inflow of pre-infirmary providers.
Gradual improvements in the pattern of defibrillators, partly based on the piece of work developing implanted versions (see below), have led to the availability of Automated External Defibrillators. These devices tin can analyse the heart rhythm by themselves, diagnose the shockable rhythms, and accuse to treat. This means that no clinical skill is required in their use, assuasive lay people to respond to emergencies effectively.
Waveform change [edit]
Until the mid 90s, external defibrillators delivered a Lown type waveform (run across Bernard Lown) which was a heavily damped sinusoidal impulse having a mainly uniphasic characteristic. Biphasic defibrillation alternates the direction of the pulses, completing one bike in approximately 12 milliseconds. Biphasic defibrillation was originally developed and used for implantable cardioverter-defibrillators. When applied to external defibrillators, biphasic defibrillation significantly decreases the free energy level necessary for successful defibrillation, decreasing the hazard of burns and myocardial harm.
Ventricular fibrillation (VF) could be returned to normal sinus rhythm in 60% of cardiac abort patients treated with a single shock from a monophasic defibrillator. Most biphasic defibrillators accept a first shock success rate of greater than 90%.[38]
Implantable devices [edit]
A further development in defibrillation came with the invention of the implantable device, known as an implantable cardioverter-defibrillator (or ICD). This was pioneered at Sinai Infirmary in Baltimore past a squad that included Stephen Heilman, Alois Langer, Jack Lattuca, Morton Mower, Michel Mirowski, and Mir Imran, with the help of industrial collaborator Intec Systems of Pittsburgh.[39] Mirowski teamed up with Mower and Staewen, and together they commenced their enquiry in 1969. However, it was xi years before they treated their first patient. Similar developmental piece of work was carried out by Schuder and colleagues at the University of Missouri.
The work was commenced, despite doubts amongst leading experts in the field of arrhythmias and sudden death. In that location was dubiousness that their ideas would ever go a clinical reality. In 1962 Bernard Lown introduced the external DC defibrillator. This device applied a direct current from a discharging capacitor through the breast wall into the heart to stop heart fibrillation.[xl] In 1972, Lown stated in the journal Circulation — "The very rare patient who has frequent bouts of ventricular fibrillation is all-time treated in a coronary care unit and is better served by an effective antiarrhythmic programme or surgical correction of inadequate coronary blood period or ventricular malfunction. In fact, the implanted defibrillator organisation represents an imperfect solution in search of a plausible and practical application."[41]
The problems to exist overcome were the pattern of a arrangement which would permit detection of ventricular fibrillation or ventricular tachycardia. Despite the lack of financial bankroll and grants, they persisted and the first device was implanted in February 1980 at Johns Hopkins Hospital past Dr. Levi Watkins Jr. assisted by Vivien Thomas. Modernistic ICDs do not require a thoracotomy and possess pacing, cardioversion, and defibrillation capabilities.
The invention of implantable units is invaluable to some regular sufferers of eye problems, although they are generally merely given to those people who take already had a cardiac episode.
People can live long normal lives with the devices. Many patients have multiple implants. A patient in Houston, Texas had an implant at the age of 18 in 1994 by the recent Dr. Antonio Pacifico. He was awarded "Youngest Patient with Defibrillator" in 1996. Today these devices are implanted into modest babies shortly after nascency.
Club and culture [edit]
As devices that tin quickly produce dramatic improvements in patient health, defibrillators are oftentimes depicted in movies, television set, video games and other fictional media. Their office, yet, is ofttimes exaggerated with the defibrillator inducing a sudden, violent jerk or convulsion past the patient. In reality, while the muscles may contract, such dramatic patient presentation is rare. Similarly, medical providers are often depicted defibrillating patients with a "flat-line" ECG rhythm (also known as asystole). This is not normal medical do, as the middle cannot be restarted by the defibrillator itself. Only the cardiac arrest rhythms ventricular fibrillation and pulseless ventricular tachycardia are ordinarily defibrillated. The purpose of defibrillation is to depolarize the entire heart all at once so that it is synchronized, effectively inducing temporary asystole, in the hope that in the absence of the previous abnormal electrical activity, the middle will spontaneously resume beating normally. Someone who is already in asystole cannot be helped by electric means, and normally needs urgent CPR and intravenous medication (and even these are rarely successful in cases of asystole). A useful illustration to remember is to think of defibrillators as power-cycling, rather than leap-starting, the heart. In that location are besides several heart rhythms that can exist "shocked" when the patient is not in cardiac arrest, such as supraventricular tachycardia and ventricular tachycardia that produces a pulse; this more-complicated procedure is known as cardioversion, non defibrillation.
In Commonwealth of australia upwards until the 1990s it was relatively rare for ambulances to carry defibrillators. This changed in 1990 later Australian media mogul Kerry Packer suffered a cardiac arrest due to a heart attack and, purely by chance, the ambulance that responded to the call carried a defibrillator. After recovering, Kerry Packer donated a large sum to the Ambulance Service of New South Wales in order that all ambulances in New South Wales should be fitted with a personal defibrillator, which is why defibrillators in Australia are sometimes colloquially called "Packer Whackers".[42]
Run into also [edit]
- Advanced cardiac life support
- Automated external defibrillator
- Ambulance
- Cardioversion
- Myocardial infarction
- Wearable cardioverter defibrillator
References [edit]
- ^ a b c d e Ong, ME; Lim, S; Venkataraman, A (2016). "Defibrillation and cardioversion". In Tintinalli JE; et al. (eds.). Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 8e. McGraw-Hill (New York, NY).
- ^ a b c d e f Kerber, RE (2011). "Chapter 46. Indications and Techniques of Electrical Defibrillation and Cardioversion". In Fuster V; Walsh RA; Harrington RA (eds.). Hurst's The Heart (13th ed.). New York, NY: McGraw-Hill – via AccessMedicine.
- ^ Werman, Howard A.; Karren, K; Mistovich, Joseph (2014). "Automated External Defibrillation and Cardiopulmonary Resuscitation". In Werman A. Howard; Mistovich J; Karren K (eds.). Prehospital Emergency Intendance, 10e. Pearson Education, Inc. p. 425.
- ^ Knight, Bradley P. Page, Richard L; Downey, Brian C (eds.). "Basic principles and technique of external electrical cardioversion and defibrillation". UpToDate . Retrieved 2019-07-24 .
- ^ Hoskins, MH; De Lurgio, DB (2012). "Chapter 129. Pacemakers, Defibrillators, and Cardiac Resynchronization Devices in Infirmary Medicine". In McKean SC; Ross JJ; Dressler DD; Brotman DJ; Ginsberg JS (eds.). Principles and Practice of Hospital Medicine. New York, NY: McGraw-Hill – via Admission Medicine.
- ^ a b c Venegas-Borsellino, C; Bangar, Dr. (2016). "CPR and ACLS Updates". In Orpello JM; et al. (eds.). Critical Care. McGraw-Colina (New York, NY).
- ^ Marenco, JP; Wang, PJ; Link, MS; Homoud, MK; Estes Iii, NAM (2001). "Improving Survival From Sudden Cardiac ArrestThe Role of the Automated External Defibrillator". JAMA. 285 (ix): 1193–1200. doi:ten.1001/jama.285.9.1193. PMID 11231750 – via JAMA Network.
- ^ "What is an automated external defibrillator? Defibrillators, cardiac arrest". 2011-06-23. Archived from the original on 2011-06-23. Retrieved 2021-11-08 .
- ^ a b "Cardiopulmonary Resuscitation (CPR): Exercise Essentials, Preparation, Technique". 2016-11-03. Archived from the original on 2016-12-07.
- ^ Nadkarni, Vinay M. (2006-01-04). "First Documented Rhythm and Clinical Outcome From In-Hospital Cardiac Arrest Amid Children and Adults". JAMA. 295 (1): 50–7. doi:10.1001/jama.295.1.fifty. ISSN 0098-7484. PMID 16391216.
- ^ Nichol, Graham (2008-09-24). "Regional Variation in Out-of-Hospital Cardiac Arrest Incidence and Outcome". JAMA. 300 (12): 1423–31. doi:x.1001/jama.300.12.1423. ISSN 0098-7484. PMC3187919. PMID 18812533.
- ^ Beaumont, E (2001). "Teaching Colleagues and the General Public nigh Automatic External Defibrillators". Medscape. Prog Cardiovasc Nurs. Archived from the original on January 23, 2017. Retrieved Dec 8, 2016.
- ^ Center for Devices and Radiological Health. "External Defibrillators - External Defibrillator Improvement Initiative Paper". www.fda.gov. Archived from the original on 2016-xi-10. Retrieved 2016-12-08 .
- ^ a b Powell, Judy; Van Ottingham, Lois; Schron, Eleanor (2016-12-01). "Public defibrillation: increased survival from a structured response organization". The Journal of Cardiovascular Nursing. 19 (6): 384–389. doi:ten.1097/00005082-200411000-00009. ISSN 0889-4655. PMID 15529059. S2CID 28998226.
- ^ a b Investigators, The Public Access Defibrillation Trial (2004-08-12). "Public-Access Defibrillation and Survival after Out-of-Hospital Cardiac Arrest". New England Journal of Medicine. 351 (7): 637–646. doi:10.1056/NEJMoa040566. ISSN 0028-4793. PMID 15306665.
- ^ Yeung, Joyce; Okamoto, Deems; Soar, Jasmeet; Perkins, Gavin D. (2011-06-01). "AED training and its touch on on skill conquering, retentivity and performance--a systematic review of alternative training methods" (PDF). Resuscitation. 82 (6): 657–664. doi:10.1016/j.resuscitation.2011.02.035. ISSN 1873-1570. PMID 21458137.
- ^ a b c Chan, Paul S.; Krumholz, Harlan M.; Spertus, John A.; Jones, Philip G.; Cram, Peter; Berg, Robert A.; Peberdy, Mary Ann; Nadkarni, Vinay; Mancini, Mary E. (2010-11-17). "Automated external defibrillators and survival subsequently in-infirmary cardiac arrest". JAMA. 304 (nineteen): 2129–2136. doi:x.1001/jama.2010.1576. ISSN 1538-3598. PMC3587791. PMID 21078809.
- ^ a b c Perkins, GD; Handley, AJ; Koster, RW; Castren, M; Smyth, T; Monsieurs, KG; Raffay, V; Grasner, JT; Wenzel, V; Ristagno, 1000; Soar, J (2015). "European Resuscitation Council Guidelines for Resuscitation 2015 Department 2. Adult basic life support and automated external defibrillation" (PDF). Resuscitation. 95: 81–99. doi:10.1016/j.resuscitation.2015.07.015. PMID 26477420. Archived (PDF) from the original on 2016-12-xx.
- ^ "Benefits of Fully Automated Defibrillators" (PDF). Physio-Control. 2011. Archived (PDF) from the original on 29 March 2012. Retrieved 12 Dec 2016.
- ^ "What is the LifeVest?". Zoll Lifecor. Archived from the original on 2008-11-21. Retrieved 2009-02-09 .
- ^ Adler, Arnon; Halkin, Amir; Viskin, Sami (2013-02-19). "Wearable Cardioverter-Defibrillators". Circulation. 127 (7): 854–860. doi:10.1161/CIRCULATIONAHA.112.146530. ISSN 0009-7322. PMID 23429896.
- ^ "What is the Departure Betwixt Adult and Pediatric Pads". AED Brands. 2018-05-xvi. Retrieved 2021-08-06 .
- ^ Jolley, Matthew; Stinstra, Jeroen; Pieper, Steve; MacLeod, Rob; Brooks, Dana; Cecchin, Frank; Triedman, John (2008). "A Computer Modeling Tool for Comparing Novel ICD Electrode Orientations in Children and Adults". Heart Rhythm. 5 (4): 565–572. doi:10.1016/j.hrthm.2008.01.018. PMC2745086. PMID 18362024.
- ^ a b Trayanova N (2006). "Defibrillation of the heart: insights into mechanisms from modelling studies". Experimental Physiology. 91 (ii): 323–337. doi:10.1113/expphysiol.2005.030973. PMID 16469820. S2CID 29999829.
- ^ Prevost J.L., Batelli F. (1899). "Some Effects of Electric Discharge on the Hearts of Mammals". Comptes Rendus de l'Académie des Sciences. 129: 1267–1268.
- ^ Lockyer, Sir Norman (1900). "Restoration of the Functions of the Heart and Central Nervous Organization after Complete Anemia". Nature. 61: 532.
- ^ Corporation, Bonnier (ane October 1933). "Pop Science". Bonnier Corporation. Retrieved 2 May 2018 – via Google Books.
- ^ "Claude Beck, defibrillation and CPR". Case Western Reserve University. Archived from the original on 2007-10-24. Retrieved 2007-06-15 .
- ^ Sov Zdravookhr Kirg. (1975). "Some results with the employ of the DPA-3 defibrillator (developed by V. Ia. Eskin and A. M. Klimov) in the treatment of terminal states". Sovetskoe Zdravookhranenie Kirgizii (in Russian). 66 (4): 23–25. doi:x.1016/0006-291x(75)90518-5. PMID half dozen.
- ^ a b "Apparatus for defibrillation or cardioversion with a waveform optimized in the frequency domain". Patents. 21 June 2006. Archived from the original on 24 September 2015. Retrieved 22 September 2014.
- ^ Гурвич Н.Л., Юньев Г.С. О восстановлении нормальной деятельности фибриллирующего сердца теплокровных посредством конденсаторного разряда // Бюллетень экспериментальной биологии и медицины, 1939, Т. VIII, № 1, С. 55-58
- ^ Gurvich NL, Yunyev GS. Restoration of a regular rhythm in the mammalian fibrillating heart // Am Rev Sov Med. 1946 Feb;three:236-9
- ^ Аппарат для дефибрилляции сердца одиночным электрическим импульсо,м in: Гурвич Н.Л. Фибрилляция и дефибрилляция сердца. Moscow, Medgiz, 1957, pp. 229-233.
- ^ Elektrická kardioverze a defibrilace, Intervenční a akutní kardiologie, 2011; ten(1)
- ^ Humphrey H H. My marathon talk with Russia'due south boss: Senator Humphrey reports in total on Khrushchev — his threats, jokes, criticism of China'southward communes New York, Time, Inc., 1959, pp. fourscore–91.
- ^ Humphrey H.H. "An of import phase of world medical research: Let's compete with U.s.a.S.R. in research on reversibility of decease." Congressional Records, October 13, 1962; A7837–A7839
- ^ "П О РТА ТИ ВН Ы Й Д Е Ф И Б Р И Л Л Я Т О Р С У Н И В Е РС А Л Ь Н Ы М ПИТАНИЕМ" Archived 2014-11-29 at the Wayback Machine (Portable defibrillator with universal power supply)
- ^ Heart Smarter: EMS Implications of the 2005 AHA Guidelines for ECC & CPR Archived 2007-06-16 at the Wayback Car pp 15-sixteen
- ^ Gold, Michael; Nisam, Seah (January 21, 2002). "Jack Lattuca". Pacing and Clinical Electrophysiology. 25 (v): 876–876. doi:x.1046/j.1460-9592.2002.t01-one-00876.x. Archived from the original on 2013-01-05 – via Wiley Online Library.
- ^ Aston, Richard (1991). Principles of Biomedical Instrumentation and Measurement: International Edition. Merrill Publishing Company. ISBN978-0-02-946562-2.
- ^ Giedwoyn, Jerzy O. (1972). "Pacemaker Failure post-obit External Defibrillation" (PDF). Circulation. 44 (2): 293. doi:x.1161/01.cir.44.ii.293. ISSN 1524-4539. PMID 5562564. S2CID 608076.
- ^ Karl Kruszelnicki (2008-08-08). "Dr Karl'southward Corking Moments In Science, Flatline and defibrillator (Part Ii)". Australian Broadcasting Corporation. Archived from the original on 2012-11-10. Retrieved 2011-12-21 .
Bibliography [edit]
- Picard, André (2007-04-27). "School defibrillators could be a lifesaver". The Globe and Mail . Retrieved 2015-07-23 .
External links [edit]
- Sudden Cardiac Arrest Foundation
- Center for Integration of Medicine and Innovative Technology
- American Ruby Cross: Saving a Life is as Easy as A-East-D
- FDA Eye Health Online: Automated External Defibrillator (AED)
Source: https://en.wikipedia.org/wiki/Defibrillation
0 Response to "what are the paddles called used to resuscitate"
Postar um comentário